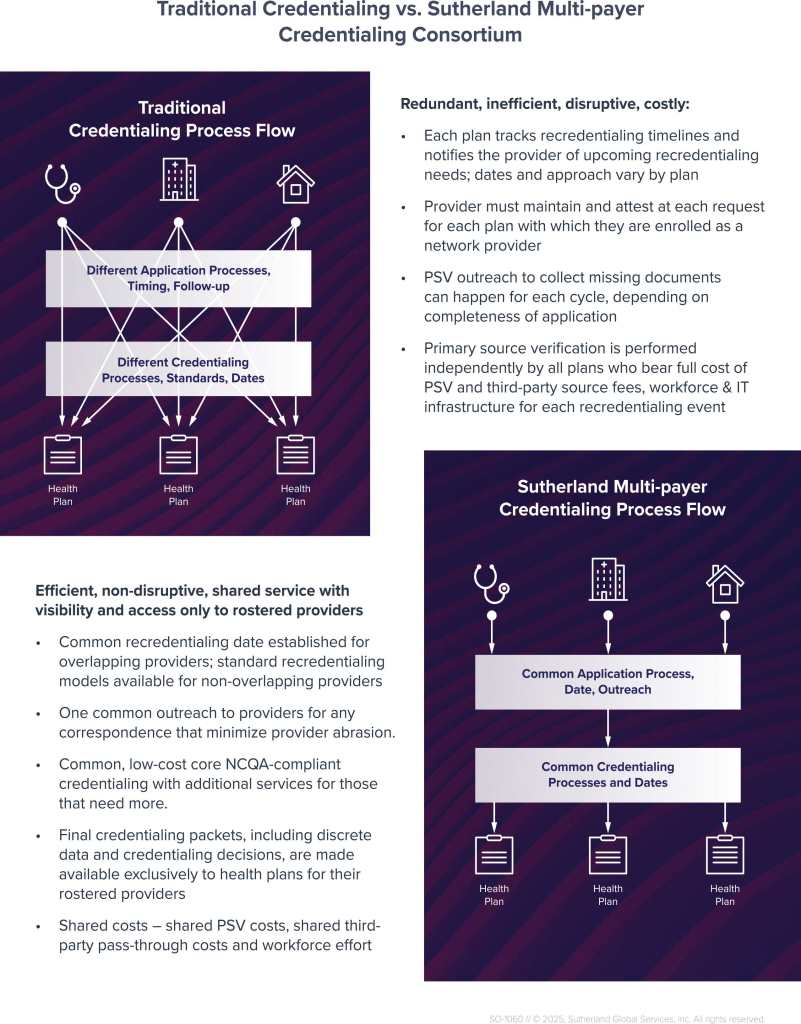
Credentialing is critical to payer operations, but traditional methods are redundant, costly, and frustrating for both health plans and providers. Each health plan independently verifies provider credentials, triggering repetitive tasks, high administrative burdens and delays in network participation.
Sutherland is reimagining that reality with MultiPayer Credentialing Consortium – a transformative shared service model that simplifies and streamlines credentialing for overlapping provider networks—without compromising compliance or control. How?
It offers a national, NCQA-certified shared services model where health plans:
- Share credentialing administration while retaining network control
- Eliminate redundancy across overlapping provider networks
- Dramatically reduce per-provider PSV and workforce costs
It’s a smarter way to credential: one schedule, one process, and secure credential packets available to all participating plans.
Key Benefits:
- Single, Simplified Credentialing Process
One outreach, one verification cycle—shared across payers - Reduced Administrative Costs
Shared PSV and third-party costs lower operational overhead. - Automated and Accelerate Credentialing
Powered by centralized scheduling, SmartCred-led automated credentialing, and dashboard tracking. - High Compliance Standards
NCQA-compliant packets with optional custom verification layers - Provider-Centric Engagement
Less abrasion, consistent communication, and improved satisfaction - Custom Dashboards & Reporting
Real-time credentialing status visibility for each health plan - Recredentialing Sync Across Plans
Reduced duplication and faster time-to-network
Let Sutherland help you eliminate redundancy and elevate the credentialing experience—at scale.