Drive Efficient Payer Operations
As the healthcare landscape continues to evolve, we help payers navigate industry challenges and deliver high-quality, cost-effective care to patients.
We offer tailored human-centric payer solutions that deliver optimized payer operations, enhanced patient experiences, and regulatory compliance.
- Improved Decision-Making. Enhance decision-making with contextual insights.
- Reduced Turnaround Time. Minimize your team’s workload and shorten turnaround time by deploying omnichannel outreach.
- Reduced Operational Costs. We help drive reduction of operational costs by as much as 30% — whether you’re a large payer, a regional health plan, or a national PPO.
Measurable Healthcare Outcomes
Reduced outreach effort
Faster turnaround time
Fewer outreach attempts
Lower operational costs
Our Solutions
Delivering seamless operations, reduced costs, and exceptional patient experiences.
Business Processes
Digital Health Solution for Payers
Data and AI
Technology Services
Regulatory Compliance and Risk Management
BPaaS
Accelerate Transformation with End-to-End Digital Engineering Solutions
Define
Strategy Blueprint
Revamp business with profound industry and technological expertise.

Design
Reimagined Experiences
Create superior experiences using a multi-lens world view.
Develop
Tailored Solutions
Build disruptive custom tech and data platforms to unlock insights.
Deploy
Market-Leading Tech
Swiftly deploy and harness bespoke technology solutions.
Drive
Innovation at Scale
Manage and optimize enterprise systems and apps at scale.
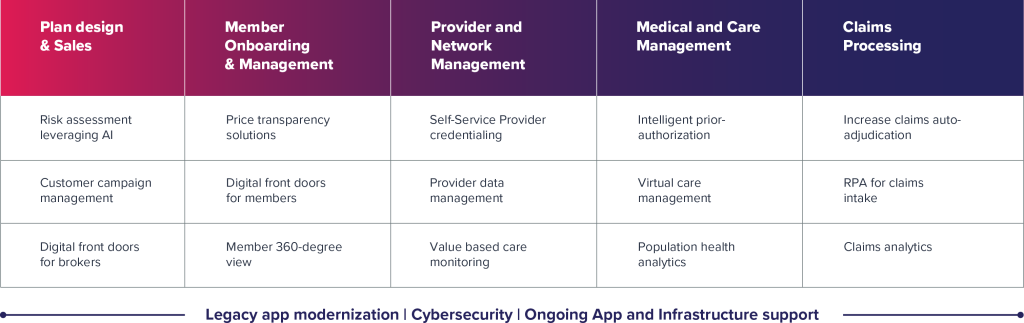
High-Impact Digital Engineering Use Cases
Healthcare Platforms
Powering innovation for your digital transformation journey
Manage large volumes of healthcare data and deliver actionable insights
SmartHealthConnect and SmartHealthAnalyticsOmnichannel outreach through our SmartCred platform reduces provider friction and cuts turnaround time
SmartCred™Roster automation, inventory management, data cleansing, and validation
Patient survey management platform for healthcare providers
Survey Management PlatformCross-Functional Platforms
Automate processes and create valuable capacity for strategic work
Robility<strong><strong><strong><strong><strong><strong>®</strong></strong></strong></strong></strong></strong>Intelligent supply chain visibility platform
eSeal<strong><strong><strong><strong><strong><strong>®</strong></strong></strong></strong></strong></strong>Smarter knowledge management for superior customer experience – powered by AI
HelpTree.AIAI-powered intelligent document processing platform
Extract.AISupercharge your automation journey with end-to-end test automation
CloudTestrAI-powered omnichannel customer experience platform
Sutherland Connect<strong><strong><strong>®</strong></strong></strong>Sophisticated AI-powered chat and voice automation for self-service interactions
Conversational AIWhy Sutherland
Improved Efficiency
Automate processes such as claims processing, billing, and payments to reduce manual work, speed up transactions, and minimize errors.
Cost Savings
Streamline operations and reduce administrative overhead to reduce costs to enable competitive pricing and optimize resource allocation.
Enhanced Member Experience
Improve customer service and drive higher member satisfaction and retention through quicker claims processing and personalized member communications.
Regulatory Compliance
Ensure adherence to laws and regulatory requirements such as HIPAA.






