In an era of rising regulatory complexity and growing provider networks, payers need a smarter, faster, and more scalable way to credential to avoid any delays.
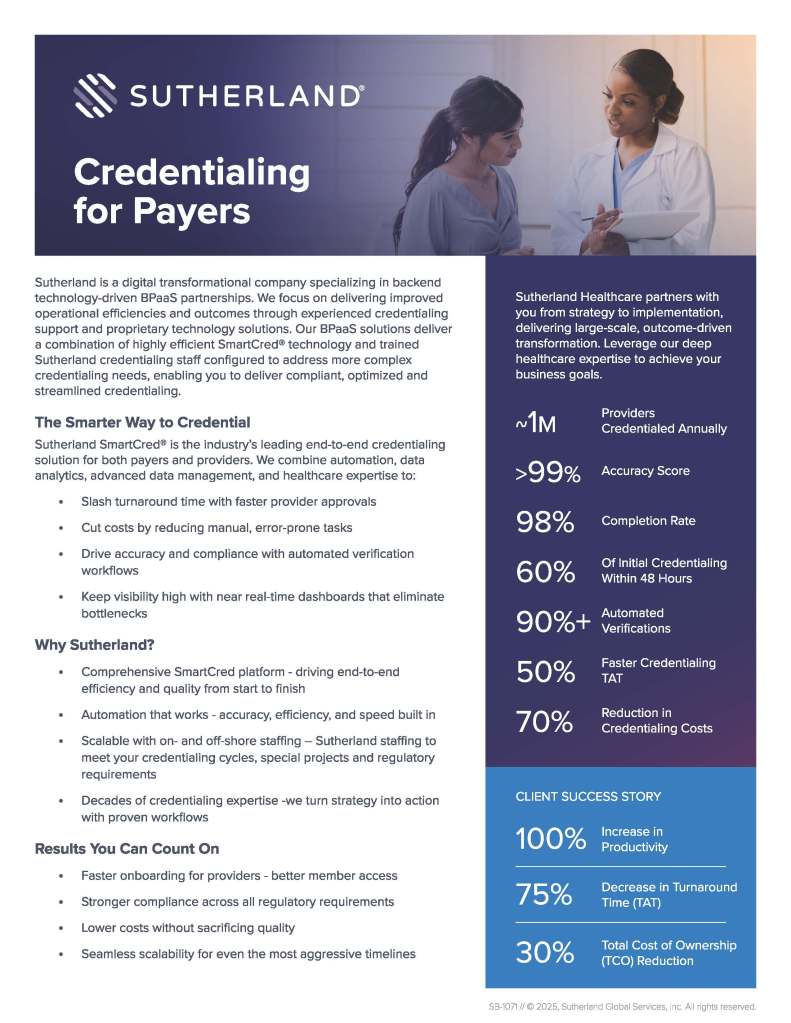
Sutherland’s Payer Credentialing solution combines advanced automation, data intelligence, and deep healthcare expertise to transform every step of the credentialing process. Powered by our SmartCred® platform and decades of credentialing experience, we help payers reduce manual tasks, improve turnaround time, and ensure compliance—all while lowering total cost of ownership. Whether you need flexible staffing, full-service CVO support, or a multi-payer shared services model, Sutherland delivers a streamlined, compliant, and outcomes-driven approach that scales with your needs.
Smarter credentialing starts here.
Key Benefits
- Faster Provider Onboarding
Accelerate approvals and improve provider and member experiences with automated workflows, intelligent data validation, and real-time dashboards that keep credentialing moving. - Improved Compliance and Accuracy
Meet and exceed NCQA, URAC, and state regulatory requirements through built-in automation, primary source verification (PSV), and 300+ business validation checkpoints. - Reduced Costs and Higher ROI
Cut manual effort and error rates, lower operational expenses, and achieve up to 70% reduction in credentialing costs with Sutherland’s BPaaS-driven delivery model. - Scalable Workforce and Technology
Leverage on- and offshore credentialing specialists and our configurable SmartCred® platform to adapt seamlessly to credentialing cycles, special projects, and market demands. - Enhanced Provider and Member Experience
Minimize provider fatigue, reduce data-collection friction, and enable faster member access to quality care through unified, automated credentialing touchpoints.